Are you interested in learning more about the K Pouch, the experience of getting one and living with one on a daily basis? Reach out to me at kpouch@reachmehere.net
I’m ready and willing to share my experience, the good, the bad and the ugly!

Are you interested in learning more about the K Pouch, the experience of getting one and living with one on a daily basis? Reach out to me at kpouch@reachmehere.net
I’m ready and willing to share my experience, the good, the bad and the ugly!

After all the complications that arose from my Total Colectomy and Rectopexy surgery, I am determined to be more prepared for my upcoming K Pouch and Proctectomy surgery, which is an even bigger surgery, with higher complication rates.
As I outlined in my previous article Total Colectomy and Rectopexy, I suffered Ileus after that surgery. Ileus is when the intestines stop pushing through food, liquids and gas, which causes a blockage that can be both painful and dangerous. In my case it meant that anytime I ate or drank anything I would throw it straight back up, which was awful and I had horrible discomfort in my abdomen. In the worst case scenario, it can cause a life threatening tear of the intestine and/or an infection in the abdomen.

The doctor’s became concerned about dehydration and malnutrition and as a result I had NasalGastric Intubation (NGI) & Total Parenteral Nutrition (TPN) put in after some time.
If you are unable to eat or drink, a nasalgastric tube will be inserted, a tube that goes in through your nose and down into your stomach. This process is known as nasalgastric intubation (NGI). During NGI, the doctor or nurse will insert a thin plastic tube through your nostril, down your esophagus, and into your stomach. Once this tube is in place, they can use it to give you food and medicine. They can also use it to remove things from your stomach. I had this done while I was awake last time and it’s not a pleasant experience! I should also tell you that having a NGI tube in is SO UNCOMFORTABLE, whilst it’s really helpful it’s terribly unpleasant.

Whilst the NGI will help me ingest some nutrients it is unlikely to meet all my nutritional needs. Therefore I will also have Total Parenteral Nutrition (TPN) which is a form of nutritional support given completely via the bloodstream, intravenously with an IV pump. TPN administers proteins, carbohydrates, fats, vitamins, and minerals directly into the blood stream. It aims to prevent and restore nutritional deficits, allowing bowel rest while supplying adequate caloric intake and essential nutrients. I had my TPN connected to a vein in my chest, I had to be very careful moving and it was quite uncomfortable but again very much worth the discomfort!

I explained my experience of having Ileus after my previous surgery to the surgeons performing my upcoming surgery and they believe I have a high risk of getting it again. Therefore, they are going to give me NGI & TPN immediately after my upcoming surgery (I will wake up with them – thankfully I won’t be awake again while they’re put in) to try to avoid the horrible discomfort I experienced last time. Whilst NGI & TPN are unpleasant, they are significantly better than Ileus and I am grateful that my new surgeons are prepared to be proactive.
As I discussed in my article Total Colectomy and Rectopexy, I have Bipolar Disorder; I also have Generalised Anxiety Disorder (GAD) and Obsessive Compulsive Disorder (OCD). If you’re interested in finding out more about my mental health experiences you can read my other blog My Bipolar Life.
Stressful events can certainly be a precursor to a depressive or manic episode and of course increase anxiety levels. For this reason, in the lead up to my surgery I will be in regular contact with my psychiatrist and with the help of my husband, family and friends, I will be keeping a close eye on my mental health.
Having said that, at the moment I am experiencing a plethora of emotions. I’m anxious one minute, excited the next, I’m optimistic then pessimistic, I’m relieved yet concerned, I’m proud of myself yet I doubt myself constantly, I’m afraid yet determined to be brave, I’m overwhelmed yet I’m coping, I’m frustrated with having to wait until February yet I want time to slow down, I’m still depressed about my current quality of life but I’m hopeful for the future and I’m lonely yet my support network grows by the day. I think all of these emotions are completely normal and not necessarily related to my mental illness.
For the surgery itself and my recovery period I will be being cared for by the resident psychiatrist at the hospital where I am having my surgery. That psychiatrist is going to liase with my psychiatrist before my surgery and throughout my recovery to ensure I get continuity of care. I am very lucky that these specialists are happy to communicate with one another for my benefit.

Also as discussed in my article Total Colectomy and Rectopexy I discovered during my recovery from that surgery that a combination of opiodes and ketamine works best for managing my pain post surgery. I also have been advised by a number of patients who have had this surgery previously, that getting an Epidural for when you wake up can help dramatically. To arrange these pain management strategies, my Surgeons have arranged for me to meet with a Pain Specialist prior to my surgery, who will order my Epidural and manage my pain medications post surgery. It’s fantastic that these arrangements are being made prior to my surgery, I’ve never had pre-care like this before.


Also prior to my surgery, I will be meeting with the Stoma Nurse again so that she can give me much more thorough information about what to expect during my recovery. I know for example that my new stoma site, or valve site, will be (temporarily) intubated constantly for at least the first few days post surgery, but I’m not yet certain when that will be removed and how I will be taught to intubate myself. The Stoma Nurse is going to tell me everything I need to know in my pre-surgery visit. She will also tell me more about what to expect in the future and any warning signs I should be aware of for complications such as Pouchitus. She is also a ward nurse and is going to discuss with me my dietary requirements and preferences for when I do begin to eat again.

On the topic of diet, I actually follow a whole foods plant based diet. This means I avoid animal products, carbohydrates and processed foods. Whilst I don’t expect to be able to follow this diet strictly in hospital, they have assured me that they will do everything possible to accommodate my preferences, which is greatly appreciated. In the lead up to my surgery, I have been ensuring that I am getting solid and varied nutrition, trying to boost my body as much as I can and be as strong and healthy for surgery as possible. This has included doing a very nutritionally packed juice cleanse which includes more than 40 different fruits and vegetables in my juice daily.

On top of following a healthy diet I also take a number of supplements, some are for vitamins and minerals normally absorbed in the large intestine (which I don’t have anymore), some are for stress and anxiety, some are to help alleviate my spasmodic pain and so forth. This is in addition to my prescribed medications.

Finally, in the lead up to my surgery my husband and I need to arrange to be able to be in Melbourne for somewhere in the vacinity of 5-7 weeks. My husband is taking carers leave from his work; our pets will be cared for by his parents and we are currently working on booking accommodation and travel. After I am discharged from the hospital we will need to remain in Melbourne for an additional three weeks to ensure that I have no post surgery complications and that I am intubating without incident, before we can head home. I will be seeing my Surgeon and the Stoma Nurse regularly throughout this time, to ensure everything is progressing as planned. Incredibly, the accommodation and travel component of this adventure are going to be almost as expensive as the surgery itself! So that’s it! Bring on February!

So after about 18 months of living with incontinence, diarrhea and pain, I had had enough, something had to change. I was booked in for more botox injections in my internal anal sphincter and pelvic floor and while I was in Brisbane for that I met with my colerectal surgeon to discuss my options. The botox didn’t work by the way.
Really the only options I was presented with were to have a Proctectomy (remove my rectum) and/or have my Ileostomy reinstated OR try a device called a Sacral Neuromodulator. A Sacral Neuromodulator is like a pacemaker for your rectum, instead of telling the nerves in your heart what to do, it tells the nerves in your rectum what to do. Compared to a Proctectomy/Ileostomy it was minor surgery, so I decided to give it a try.
The Sacral Neuromodulator was implanted for a trial period of two weeks. The electrode was implanted into my spine and I wore the actual machine on a belt around my waist. The cord came out of my back and was connected to the machine and I had a remote control to change the settings/try different settings. The aim was to reduce the number of times I was going to the toilet/having accidents and hopefully (although much less likely) reduce my pain levels. Unfortunately after 2 weeks and trying all the different settings and strengths available I had no improvement in continence or diarrhea and I was in fact in more pain. So the trial was aborted and the Sacral Neuromodulator was removed. I was very disappointed, I had really had my hopes up and now my only realistic options left were major surgery.
BUT my husband in his infinite wisdom (and I mean that wholeheartedly) was not satisfied that the Proctectomy and Ileostomy could be the only options available to me, so he began researching online for alternatives and he found one! The K Pouch (otherwise known as a Kock Pouch or BCIR). But was it available in Australia?!
We started researching and I started trawling Facebook and I found a few groups of people having this surgery overseas. I found practically nothing regarding this surgery being performed in Australia. On the other hand, it has been being done in the USA and Europe for decades. Eventually, through luck, I came across a girl who had had the surgery in Australia! She was only the third person to have it done here, which was worrisome, but she was lovely and filled me in on everything I needed to know to get me started. Starting with the contact details of the surgeons who are doing it here in Australia.
So I contacted the surgeons (there are 2 of them who work as a team) and I arranged a Skype consultation with one of them, because they operate out of Melbourne. I created an extensive and exhaustive list of questions and when the day came all my questions were answered and more and it became clear that this was a very viable alternative to having my Ileostomy reinstated.
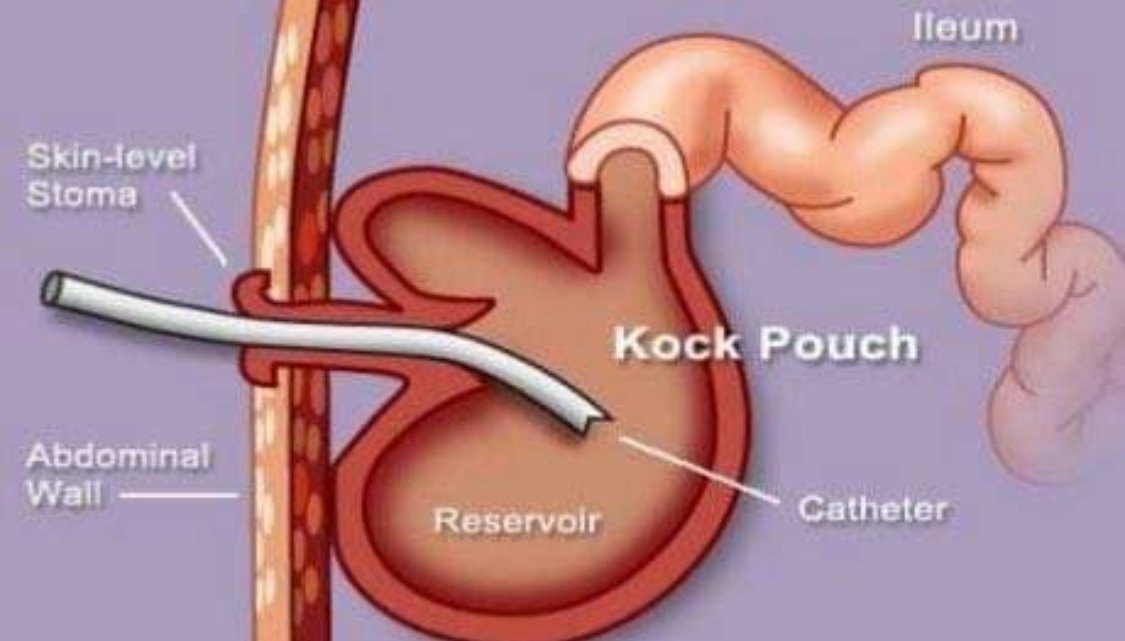
The K Pouch is an internal ileostomy, formed out of a few feet of your small intestine. It is connected to a valve on your belly and you empty it by intubating with a hose and allowing the waste to pour out of the hose into the toilet.



After my Skype appointment, I was definitely interested in finding out if I was a candidate for this surgery and to do that we had to travel to Melbourne. In Melbourne we would meet both the surgeons and the stoma nurse and I would undergo exploratory surgery to determine if I was a candidate.
This was a major undertaking, drive 4 hours to Brisbane, drop our puppies off at Dans parents then go to the airport and fly interstate to Melbourne. We stayed in a hotel on the same block as the hospital and then spent the next 10 days in Melbourne. First we met with both the surgeons, then I had my surgery, then we met with the primary surgeon again to get my results. It was determined that I’m a good candidate and that it would be worthwhile to have a Proctectomy at the same time in the hope that it will stop my pain, although there’s no guarantee as it may be nerve pain which won’t be helped by a Proctectomy but it’s worth a try. I then met with the stoma nurse, which was very informative on a practical day to day, living with a K Pouch level. And finally I booked in my surgery for 16 February 2019!
I should note here that this is MAJOR surgery, even bigger than getting my ileostomy reinstated. We will be in Melbourne for seven weeks minimum. It is a cut from your breast bone to your pelvic bone plus other incisions, over 1000 stitches all said and done. I need to be well prepared for this surgery and that will be the topic of my next article. I also want to explain that these surgeons both trained in the USA for over a decade doing these surgeries and surgeries related to complications of the K Pouch (the complication rates are relatively high). I will be the fourth person to have this surgery in Australia, that I know of.
As a result of my experiences, having so much trouble finding any information about this surgery in Australia, I created a Facebook group called K Pouch Australia. A place to find information about getting a K Pouch in Australia from people who have already had a K Pouch or BCIR or are medical professionals. Also a place for family and friends of people getting a K Pouch to gain insight into the procedure. Feel free to invite anyone you feel can benefit the group or benefit from the group to join! To join go to: https://www.facebook.com/groups/2303404103235641/
This is perhaps the hardest article for me to write for a few reasons; it’s my current life, it’s embarrassing and I feel that I might be judged for it.
At the moment I go to the toilet about every hour and a half while I’m awake plus a few times through the night, 11 times a day on average. If it weren’t for my husband installing a bidet in our house I would have severe butt burn (which I get whenever we have to travel to visit family or go to medical appointments). When I do get bad butt burn I treat it with a topical cream called Calmoseptine, which eases the burn and helps the skin heal. But with the bidet I am usually spared this problem, it actually washes and air dries my bottom for me to save wiping with toilet paper (that feels like sand paper if you use it often enough).


The consistency of my output is diarrhea, permanently, despite taking 8 gastrostop (an anti-diarrhea medication) a day and 2 tablespoons of psyllium husk (a natural fiber supplement that thickens the stool) . I also structure my diet to try to thicken my output, but more about my diet in a future article.


I should explain here that my diarrhea is because I don’t have a large intestine which removes the water from your stool. My output varies from water to toothpaste at the very best. The upside of this is that it doesn’t take long to go to the toilet the downside is that I don’t always make it to the toilet. In fact sometimes I get no warning at all. So yes, I’m incontinent and as embarrassing as it is to admit I have to live in diapers/pullups/nappies. This is embarrassing obviously but also expensive and impractical, they are bulky and uncomfortable and show under your clothes. It may sound vein, but I really struggle with the constant worry that people can tell that I’m wearing a diaper. This is probably not helped by my anxiety disorder, a side effect of my bipolar disorder (www.mybipolarlife.net).

And then there’s the awful occurrence of an accident out in public, which has me running to the closest restroom with my emergency bag, to clean myself up and put on a fresh diaper, and in the worst case scenario change my clothes because I’ve overflowed my nappy. Even when I don’t have an accident, when I am out in public I always have to be aware of the closest restroom because I may not get a lot of warning when it’s time to go.
Since the days of having my ileostomy, I have struggled with intermittent, internal anal sphincter and pelvic floor spasms, which are excruciating. Some ladies equivalate the pain to a childbirth contraction. In recent months this has become a permanent part of my life.

Before turning to drastic measures to ease this pain, I had a number of sessions with a specialist pelvic floor physiotherapist. She taught me (and my husband) quite a few techniques for relaxing the relevant muscles through special exercises, we still use these techniques to this day when the pain is unbearable, they help ease it off a little but can occasionally make it worse.
Later, I was treated with botox injections in my internal anal sphincter and pelvic floor and this would give me relief for about 2-3months. Recently however the botox has stopped working. I now take 12 magnesium phosphate tablets a day (which help with muscle spasm), plus 6 valium (muscle relaxants and anti-anxiety medication also known as diazepam) and 4 endone (a strong opiate painkiller, also known as oxycodone), just to bring the pain down to a manageable level. If I have to travel long distances in the car or do a lot of walking/movement I require more medication.



I hate being reliant on addictive medications, but it is a necessary evil to be able to live in relative comfort at this point in my life. I consult closely with my psychiatrist, my GP and my chemist to manage my use of these medications and it is very definitely a short term solution to the problem, the long term solution will be the topic of my next article.


So I was back at my Colerectal Surgeon’s office to discuss my long term options. Once again I had a few options to choose from. I could keep my bag and continue on as is, putting up with the aggravating factors and the self esteem issues. OR I could undo my loop ileostomy and go back to living with a Slow Transit Megacolon and try to manage my quality of life as best I could with laxatives, fiber and diet, with the option of having my prolapsed rectum repaired (a Sutured Rectopexy) OR I could take drastic measures and have my large intestine removed (a Total Colectomy) and have my prolapsed rectum repaired (a Sutured Rectopexy) and then have my loop ileostomy closed off and my small intestine connected directly to my rectum (Ileorectal Anastomosis). Once again I chose option 3, but in retrospect I really didn’t understand what I was signing up for and I’ll explain why.
I understood of course that this was major surgery, I was going to be in the hospital for a couple of weeks and recovery would be slow and painful. I feel like I should also mention here that I have Bipolar Disorder (www.mybipolarlife.net) and so I have the added stress of trying not to destabilize my bipolar while I’m going through physical health challenges.
What I didn’t anticipate was the number of complications that would eventuate and lead to additional surgeries. The worst of these was something called Ileus, which is where my small intestine stopped working for a week due to the stress it had undergone in the surgery. This led to me not being able to eat or drink anything without it coming straight back up and eventually meant I had to get NasalGastric Incubation (NGI) and Total Parenteral Nutrition (TPN) both very uncomfortable and awkward and neither particularly helpful! In fact they were both removed after a number of days and my body was allowed to heal itself.
That whole week was atrocious, being hooked up to so many machines and medications and so forth was only made worse by the complete lack of communication from my surgeon. While I’m sure he had my best interests at heart and while I’m sure he had contingency plans in mind for the various possible outcomes, he did not communicate any of this to me, which caused me extreme anxiety (which is exacerbated by my bipolar disorder).
Towards the end of my second week in hospital, when I had already had two surgeries and was still not doing well, I and my husband were starting to get very frustrated. We hadn’t seen a doctor in days, the nurses couldn’t tell us what was happening or what would be done about my poor condition, we were at a loss. My husband then spoke to the head nurse, who couldn’t help and then to the ward nurse, at this point he threatened to enact Ryan’s Rule (which I’ll tell you more about shortly) and like magic things began to happen. A doctor arrived, assessed me and booked me for my third surgery.
The Ryan’s Rule came about because a poor young boy died in North Queensland because he wasn’t properly cared for, his parents, after his death, petitioned the government to create the Ryan’s Rule so that people who feel their legitimate concerns are being ignored can demand a revision of their care plan, we thank Ryan’s parents for petitioning for this rule, we have used it a number of times over the years, with excellent outcomes.
One thing I learned during this time was the importance of the cocktail of drugs you are on. At first my pain medications were only opiodes, when this clearly wasn’t cutting it, they added ketamine and the combination of the opiodes and ketamine together was fantastic, my pain became bearable and I began to want to recover faster, move around more, get better quicker.
The rest of my recovery was relatively smooth and involved starting to go to the toilet again, gradually reintroducing more and more solid foods and physiotherapy. There was however, no psychological support provided, having said that I could have called my own psychiatrist if need be.
All in all I was in hospital for about three weeks and had two additional surgeries for adhesions and infections. They really took good care of me, despite the lack of communication. By the time I was ready to be discharged I was moving around fairly well, eating decently and going to the bathroom regularly and without incident, with the exception of a few accidents. I felt things were going fairly well.
Going home (or more correctly to my in-laws in Brisbane) was helped greatly by my Mother-in-law caring for me in every way possible, including helping me change my dressings especially the one where my stoma used to be which was now a gaping hole in my stomach! They didn’t sew it shut, so we got to watch it magically close itself over the next few weeks! I was still in a fair amount of pain during this time which was managed with opiodes and I struggled for the first few weeks to get up and down the stairs in the house. My diet was kind of like baby food, everything soft and mushy and I had some trouble sleeping because of the pain if I turned over. But really for the most part I was doing well.
What I should have anticipated (but didn’t) was how bad my diarrhea would be and the fact that I would be incontinent. Over the next 18 months I would try almost everything I could think of to thicken my stool and encourage my rectum to work properly to no avail. But more about that in my next article.
So having been diagnosed with Slow Transit Megacolon my colerectal surgeon was interested to see whether my rectum had been damaged by years of chronic constipation. So I was sent for more demeaning and embarrassing tests and it was established that my rectum was in fact prolapsed. With the combination of diagnoses, I had to make a decision on the best course of action.
My options as they were presented to me were to do nothing and keep trying to manage my symptoms with medications (laxatives and fiber) and dietary changes (that would improve my stool consistency but not my general health) OR have a total colectomy (removal of the large intestine) and a rectopexy (repair of the rectum) OR get a temporary loop ileostomy and buy myself some time to decide about major surgery whilst improving my general health with diet and exercise. I chose option 3!
It was still fairly major surgery and it meant living with an ileostomy bag, but it meant a fast improvement in the quality of my life and my health. So we went ahead with that surgery and boy did my life change!
I should probably explain that an ileostomy bypasses your large intestine, what this means is that your ‘output’ is far more liquidy because it’s the large intestine that removes the liquid from your stool. So I went from being chronically constipated to having liquid output overnight, quite a drastic change and a mind warp!
I had to get used to emptying my bag frequently and making sure I didn’t get caught out without access to a bathroom. I also had to adjust to physically wearing the bag and the many practicalities of that, skin irritation from the glue, leaks, problems with fit and hold, changing the bag regularly, there was a plethora of logistical problems that needed to be managed. Thankfully I’m married to a very practical fellow who came up with creative solutions to almost all the problems I faced.
My life got back on track, my diet was somewhat limited to avoid blockages, but nothing unmanageable, I was able to exercise again and I could do almost anything a normal person could do. But I did suffer quite a bit of skin irritation which was painful and I did suffer some self esteem issues from having the bag, but it was only a temporary solution so I coped with those issues.
After having the Ileostomy for 18 months it was time to start making some long term decisions and so I went back to my colerectal surgeon!




I have always had slow bowels, but I didn’t know it for a long time, I thought it was normal to only do a poo once a week. Slowly over time once a week became ten days, became 2 weeks and so on. About 5 years ago, I was diagnosed with Slow Transit Megacolon, but let me explain how I got to that diagnosis.
My large intestine had stopped working, the muscles were dead, but I didn’t know it. This led to chronic constipation and regular bowel compactions. I was living on laxatives and would often go up to a month without doing a poo. I was extremely uncomfortable at best and in agony at worst, but couldn’t take any pain relief because it would lead to further constipation. I had lost my appetite and was unable to exercise or live a full life because of my ill health. I was doing regular colonoscopy preparations at home (for example Moviprep) to clear my bowels out as best I could.
When that didn’t work I would have to go to the hospital to have them clear my bowels. I should note here that I live in a small country town, 4 hours west of the closest city, so would have to travel 4 hours to the hospital, usually in agony. I would then get cleared out and sent home, only to end up back there a month later. Those hospital visits were demeaning and depressing often losing complete control of my bowels in the worst places, I remember distinctly losing my bowels in the lift one time on the way back to my room. After about 10 hospital clean outs I sought out the help of a colerectal surgeon and this led to a plethora of also demeaning and depressing tests and eventually a diagnosis of Slow Transit Megacolon.